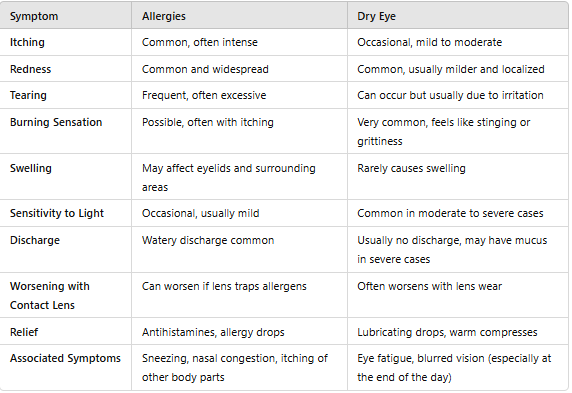
Both dry eye syndrome and eye allergies can cause discomfort, but each condition has specific characteristics that can help you identify the underlying cause. Here’s a guide to typical symptoms and tips for recognizing whether they’re likely from dry eye or allergies.
Dry eye symptoms
Dry eye syndrome occurs when your eyes don’t produce enough tears or the tears drain too quickly. Tears are crucial for keeping the eyes lubricated, providing nutrients, and protecting them from irritants. When this natural moisture is lacking, eyes can feel dry, scratchy, and sore. Common causes of dry eye include:
- Gritty or Burning Sensation: Dry eye typically feels like there’s something in the eye, often described as a gritty or sandy feeling.
- Blurred Vision: Dry eye can lead to occasional blurry vision that clears with blinking or eye drops.
- Sensitivity to Light: People with dry eyes are often more sensitive to bright lights or glare.
- Less Tear Production: Unlike allergies, dry eye may result in a lack of tears, causing discomfort without excessive tearing.
- Worsens with Screens or Dry Environments: Symptoms may worsen in air-conditioned rooms, windy conditions, or after prolonged screen use.
Allergy symptoms
Eye allergies, also known as allergic conjunctivitis, occur when the eyes react to allergens like pollen, dust, pet dander, or mold. When these allergens make contact with the eye’s surface, the immune system releases histamines, causing symptoms like:
- Intense Itching: Allergies often cause a persistent urge to rub the eyes due to itching. If your eyes don’t itch, your symptoms may be caused by another eye infection
- Redness and Swelling: Allergic reactions commonly lead to visible redness and puffiness around the eyes. Some people develop dark circles under their eyes, often referred to as allergic dark circles.
- Watery Eyes: Allergies may cause excessive tearing as the body tries to wash out allergens. You may be tempted to wipe away the tears because of the pain, which can make the redness worse. It may get hot.
- Runny Nose or Sneezing: Allergies often coincide with other symptoms, like nasal congestion or sneezing.
- Triggered by Exposure: Symptoms tend to flare up in response to allergens like pollen, dust, pet dander, or mold.
Diagnosis
When your eyes feel irritated, red, or itchy, it can be challenging to know if the problem is dry eye syndrome or an allergic reaction. While the symptoms can overlap, the underlying causes and treatments for these conditions differ significantly. Here’s an overview of how eye doctors diagnose dry eye and allergies, the tests involved, and what you can expect during your visit.
How dry eye is diagnosed?
If dry eye syndrome is suspected, several specialized tests may be performed to assess tear production, tear film quality, and any underlying inflammation.
- Schirmer Test: This simple test measures tear production. A small strip of paper is placed under your lower eyelid, and after a few minutes, the moisture level on the strip indicates how much tear your eyes produce. Low moisture levels may suggest dry eye.
- Tear Breakup Time (TBUT): This test evaluates the stability of your tear film. Your eye doctor will place a dye (often fluorescein) in your eye and use a special light to observe how quickly the tear film “breaks up” on the eye’s surface. A shorter breakup time indicates unstable tears, a common sign of dry eye.
- Osmolarity Test: By measuring the salt concentration in your tears, this test helps determine whether your tear film is balanced or hyperosmolar (too salty). High osmolarity is a common indicator of dry eye.
- Meibography: This imaging test examines the health of your meibomian glands, which produce oils that prevent tears from evaporating too quickly. Dysfunction in these glands is a leading cause of evaporative dry eye.
How allergies are diagnosed?
For those with suspected eye allergies, the focus shifts to identifying the specific allergens causing the immune response and confirming allergic conjunctivitis.
- Conjunctival Examination: The doctor may use a slit lamp (a specialized microscope) to examine the surface of the eye and the conjunctiva (the clear membrane covering the white part of the eye). Signs of redness, swelling, or tiny bumps on the conjunctiva (papillae) suggest an allergic reaction.
- Allergy Testing: If the cause of the allergy isn’t clear, your doctor may refer you to an allergist for skin testing to identify specific allergens. Skin prick tests or blood tests can reveal whether you’re allergic to common triggers like pollen, dust, pet dander, or mold.
- Eosinophil Staining: This test involves gently swabbing the inside of the eyelid to collect a sample of the conjunctiva, which can be examined for eosinophils (a type of white blood cell commonly found in allergic reactions). Elevated eosinophil levels help confirm an allergic response.
- Tear Analysis: Similar to dry eye tests, a tear sample may be taken to analyze for specific proteins, enzymes, or markers associated with inflammation or allergies. High levels of certain markers can indicate an allergic reaction rather than dry eye.
Treatment options
Dry eye syndrome and eye allergies require different treatments due to their distinct causes. Understanding the difference between dry eyes vs. allergies is essential for effective relief. Dry eye is generally caused by insufficient tear production or poor tear quality, while eye allergies are an immune response triggered by allergens like pollen or pet dander. Accurately diagnosing dry eyes vs. allergies helps ensure effective treatment and long-lasting relief.
Here’s an overview of the treatment options available for both dry eye and allergies, from simple over-the-counter solutions to advanced prescription therapies.

Dry eye treatment
- Artificial Tears and Lubricating Eye Drops: Artificial tears are a first-line treatment for dry eye. They help moisten the eyes and relieve pain. If you need to use drops several times a day to avoid further irritation, look for preservative-free options like Gel drops and ointments help in the long run by creating a protective layer on the surface of the eye. It is used at night to help with dryness in the morning.
- Prescription Medications: Anti-inflammatory eye drops such as cyclosporine (Restasis) and lifitegrast (Xiidra) can reduce inflammation, increase tear production, and relieve dry eye symptoms. In cases of severe inflammation, short-term use of corticosteroid eye drops can relieve symptoms. Because of the strong side effects, this drug is used under close supervision.
- Advanced Treatments: Punctal plug that is inserted into the tear duct to slow the flow of tears and keep the eye moist for longer. For those who suffer from evaporative dry eye, lipid eye drops increase moisture and stabilize the oily layer of the tear film. Some eye doctors offer light-based therapies and manual gland expression to help treat meibomian gland dysfunction, which is a common cause of evaporative dry eye.
Allergies treatment
Treatment aims to reduce the immune response to allergens. Antihistamine drops, cold compresses, and avoidance of triggers are effective for symptom relief.
- Avoid allergies: Avoiding irritants is key to managing eye allergies. This means staying indoors during the pollen season, using an air purifier, and cleaning areas exposed to dust or pet waste. Wearing sunglasses outside can prevent allergens like pollen from getting in your eyes, and using hypoallergenic bedding can reduce exposure indoors.
- Oral antihistamines: For people with eye and nasal allergy symptoms, oral antihistamines (such as cetirizine, loratadine, or fexofenadine) can relieve more general symptoms. However, these medications can sometimes make dry eye worse, so they should be used with caution in people with dry eye.
- Cold Compresses: Keeping the eyes dry can reduce the swelling, redness and itching associated with allergies. This simple, drug-free method can relieve mild symptoms.
Prevention and lifestyle tips
Managing dry eye and eye allergies can be challenging, especially as both conditions are often triggered by everyday factors like weather, screens, and allergens. However, with a few practical tips, you can reduce symptoms and help keep your eyes comfortable. Here’s how to protect your eyes from common triggers and manage both conditions daily.
Preventing dry eye
If you suffer from dry eyes, take note of the situations that tend to trigger your symptoms. By identifying these triggers, you can find ways to avoid them and reduce the likelihood of experiencing discomfort. For example:
- Create a Comfortable Environment: The environment around you can have a huge impact on eye health. Small changes in your environment can have a big impact on reducing dry eyes and allergy symptoms like using humidifier, Limiting use of Fan and Air Conditioner, avoiding air blowing in your eyes.
- Stay Hydrated: Staying well-hydrated supports tear production. Aim for at least eight glasses a day, especially if you experience dry eye symptoms.
- Proper contact lens care: It is essential in preventing dry eye by ensuring that lenses remain clean, hydrated, and free from allergens. Regular cleaning and disinfecting of contact lenses help remove buildup of debris, proteins, and bacteria that can irritate the eyes and worsen dryness.
Preventing allergies
If you have eye allergies, managing exposure to allergens is key. These tips can help reduce contact with common triggers:
- Keep Windows Closed During High-Allergen Seasons: If you’re prone to eye allergies, keeping windows shut during peak pollen times, especially in spring and fall, can help reduce allergen exposure.
- Exposure to the outdoors: Wearing sunglasses acts as a physical barrier, preventing pollen and dust from entering your eyes. Wraparound sunglasses provide even better protection. During high-pollen days, limit outdoor activities or plan them for later in the day when pollen counts tend to be lower.
- Increase air humidity. In winter, a humidifier can add moisture to dry the indoor air.
Conclusion
Frequently Asked Questions